Medicare Benefit – the industrial different to conventional Medicare – is drawing down federal well being care funds, costing taxpayers an additional 22% per enrollee to the tune of US$83 billion a yr.
Medicare Benefit, also called Half C, was supposed to save lots of the federal government cash. The competitors amongst non-public insurance coverage firms, and with conventional Medicare, to handle affected person care was meant to provide insurance coverage firms an incentive to search out efficiencies. As an alternative, this system’s fee guidelines overpay insurance coverage firms on the taxpayer’s dime.
We’re well being care coverage specialists who research Medicare, together with how the construction of the Medicare fee system is, within the case of Medicare Benefit, working in opposition to taxpayers.
Medicare beneficiaries select an insurance coverage plan after they flip 65. Youthful folks also can turn into eligible for Medicare as a result of continual situations or disabilities. Beneficiaries have a wide range of choices, together with the normal Medicare program administered by the U.S. authorities, Medigap dietary supplements to that program administered by non-public firms, and all-in-one Medicare Benefit plans administered by non-public firms.
Industrial Medicare Benefit plans are more and more well-liked – over half of Medicare beneficiaries are enrolled in them, and this share continues to develop. Persons are attracted to those plans for his or her additional advantages and out-of-pocket spending limits. However as a result of a loophole in most states, enrolling in or switching to Medicare Benefit is successfully a one-way avenue. The Senate Finance Committee has additionally discovered that some plans have used misleading, aggressive and probably dangerous gross sales and advertising and marketing techniques to extend enrollment.
Baked into the plan
Researchers have discovered that the overpayment to Medicare Benefit firms, which has grown over time, was, deliberately or not, baked into the Medicare Benefit fee system. Medicare Benefit plans are paid extra for enrolling individuals who appear sicker, as a result of these folks usually use extra care and so could be costlier to cowl in conventional Medicare.
Nonetheless, variations in how folks’s diseases are recorded by Medicare Benefit plans causes enrollees to look sicker and costlier on paper than they’re in actual life. This subject, alongside different changes to funds, results in overpayment with taxpayer {dollars} to insurance coverage firms.
A few of this extra cash is spent to decrease value sharing, decrease prescription drug premiums and enhance supplemental advantages like imaginative and prescient and dental care. Although Medicare Benefit enrollees might like these advantages, funding them this manner is dear. For each additional greenback that taxpayers pay to Medicare Benefit firms, solely roughly 50 to 60 cents goes to beneficiaries within the type of decrease premiums or additional advantages.
As Medicare Benefit turns into more and more costly, the Medicare program continues to face funding challenges.
In our view, to ensure that Medicare to outlive long run, Medicare Benefit reform is required. The way in which the federal government pays the non-public insurers who administer Medicare Benefit plans, which can appear to be a black field, is vital to why the federal government overpays Medicare Benefit plans relative to conventional Medicare.
Paying Medicare Benefit
Personal plans have been part of the Medicare system since 1966 and have been paid by means of a number of totally different programs. They garnered solely a really small share of enrollment till 2006.
The present Medicare Benefit fee system, applied in 2006 and closely reformed by the Inexpensive Care Act in 2010, had two coverage objectives. It was designed to encourage non-public plans to supply the identical or higher protection than conventional Medicare at equal or lesser value. And, to verify beneficiaries would have a number of Medicare Benefit plans to select from, the system was additionally designed to be worthwhile sufficient for insurers to entice them to supply a number of plans all through the nation.
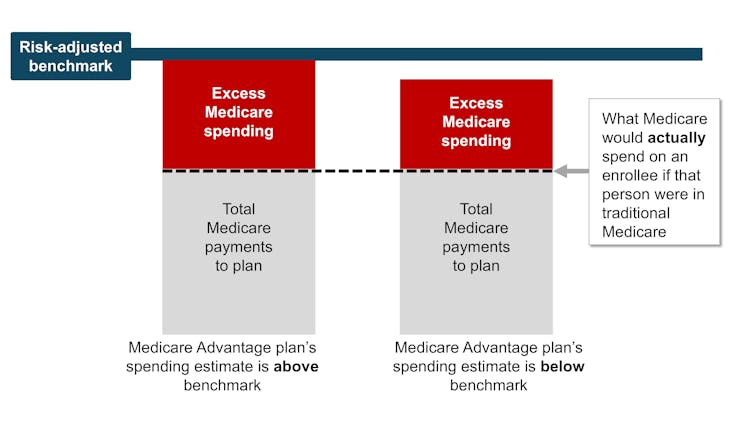
To perform this, Medicare established benchmark estimates for every county. This benchmark calculation begins with an estimate of what the government-administered conventional Medicare plan would spend on the common county resident. This worth is adjusted primarily based on a number of elements, together with enrollee location and plan high quality rankings, to provide every plan its personal benchmark.
Medicare Benefit plans then submit bids, or estimates, of what they count on their plans to spend on the common county enrollee. If a plan’s spending estimate is above the benchmark, enrollees pay the distinction as a Half C premium.
Most plans’ spending estimates are beneath the benchmark, nevertheless, which means they challenge that the plans will present protection that’s equal to conventional Medicare at a decrease value than the benchmark. These plans don’t cost sufferers a Half C premium. As an alternative, they obtain a portion of the distinction between their spending estimate and the benchmark as a rebate that they’re speculated to go on to their enrollees as extras, like reductions in cost-sharing, decrease prescription drug premiums and supplemental advantages.
Lastly, in a course of referred to as danger adjustment, Medicare funds to Medicare Benefit well being plans are adjusted primarily based on the well being of their enrollees. The plans are paid extra for enrollees who appear sicker.
Samantha Randall at USC, CC BY-ND
Principle versus actuality
In concept, this fee system ought to save the Medicare system cash as a result of the risk-adjusted benchmark that Medicare estimates for every plan ought to run, on common, equal to what Medicare would truly spend on a plan’s enrollees if that they had enrolled in conventional Medicare as a substitute.
In actuality, the risk-adjusted benchmark estimates are far above conventional Medicare prices. This causes Medicare – actually, taxpayers – to spend extra for every one that is enrolled in Medicare Benefit than if that individual had enrolled in conventional Medicare.
Why are fee estimates so excessive? There are two fundamental culprits: benchmark modifications designed to encourage Medicare Benefit plan availability, and danger changes that overestimate how sick Medicare Benefit enrollees are.
Samantha Randall at USC, CC BY-ND
Benchmark modifications
Because the present Medicare Benefit fee system began in 2006, policymaker modifications have made Medicare’s benchmark estimates much less tied to what the plan spends on every enrollee.
In 2012, as a part of the Inexpensive Care Act, Medicare Benefit benchmark estimates obtained one other layer: “quartile changes.” These made the benchmark estimates, and due to this fact funds to Medicare Benefit firms, increased in areas with low conventional Medicare spending and decrease in areas with excessive conventional Medicare spending. This benchmark adjustment was meant to encourage extra equitable entry to Medicare Benefit choices.
In that very same yr, Medicare Benefit plans began receiving “high quality bonus funds” with plans which have increased “star rankings” primarily based on high quality elements resembling enrollee well being outcomes and take care of continual situations receiving increased bonuses.
Nonetheless, analysis exhibits that rankings haven’t essentially improved high quality and will have exacerbated racial inequality.
Even earlier than absolutely considering danger adjustment, latest estimates peg the benchmarks, on common, as 8% increased than common conventional Medicare spending. Because of this a Medicare Benefit plan’s spending estimate might be beneath the benchmark and the plan would nonetheless receives a commission extra for its enrollees than it could have value the federal government to cowl those self same enrollees in conventional Medicare.
Overestimating enrollee illness
The second main supply of overpayment is well being danger adjustment, which tends to overestimate how sick Medicare Benefit enrollees are.
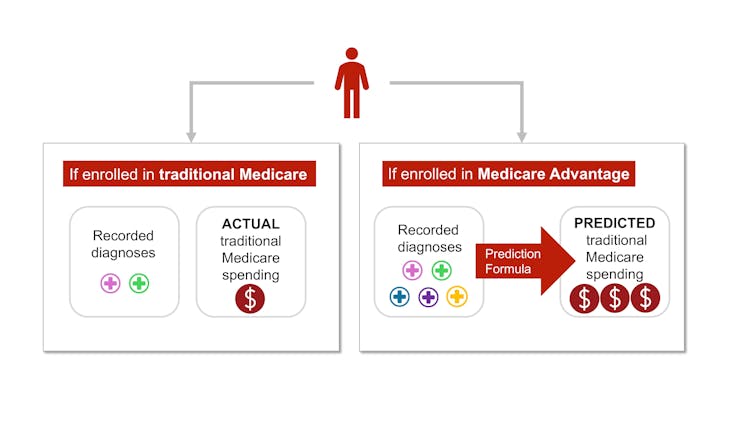
Every year, Medicare research conventional Medicare diagnoses, resembling diabetes, melancholy and arthritis, to grasp which have increased therapy prices. Medicare makes use of this data to regulate its funds for Medicare Benefit plans. Funds are lowered for plans with decrease predicted prices primarily based on diagnoses and raised for plans with increased predicted prices. This course of is named danger adjustment.
However there’s a vital bias baked into danger adjustment. Medicare Benefit firms know that they’re paid extra if their enrollees appear extra sick, in order that they diligently make certain every enrollee has as many diagnoses recorded as attainable.
This may embrace authorized actions like reviewing enrollee charts to make sure that diagnoses are recorded precisely. It will possibly additionally sometimes entail outright fraud, the place charts are “upcoded” to incorporate diagnoses that sufferers don’t even have.
In conventional Medicare, most suppliers – the exception being Accountable Care Organizations – should not paid extra for recording diagnoses. This distinction signifies that the identical beneficiary is prone to have fewer recorded diagnoses if they’re enrolled in conventional Medicare reasonably than a personal insurer’s Medicare Benefit plan. Coverage specialists consult with this phenomenon as a distinction in “coding depth” between Medicare Benefit and conventional Medicare.
Samantha Randall at USC, CC BY-ND
As well as, Medicare Benefit plans typically attempt to recruit beneficiaries whose well being care prices shall be decrease than their diagnoses would predict, resembling somebody with a really delicate type of arthritis. This is named “favorable choice.”
The variations in coding and favorable choice make beneficiaries look sicker after they enroll in Medicare Benefit as a substitute of conventional Medicare. This makes value estimates increased than they need to be. Analysis exhibits that this mismatch – and ensuing overpayment – is probably going solely going to worsen as Medicare Benefit grows.
The place the cash goes
Among the extra funds to Medicare Benefit are returned to enrollees by means of additional advantages, funded by rebates. Additional advantages embrace cost-sharing reductions for medical care and pharmaceuticals, decrease Half B and D premiums, and further “supplemental advantages” like listening to aids and dental care that conventional Medicare doesn’t cowl.
Medicare Benefit enrollees might get pleasure from these advantages, which might be thought-about a reward for enrolling in Medicare Benefit, which, not like conventional Medicare, has prior authorization necessities and restricted supplier networks.
Nonetheless, based on some coverage specialists, the present technique of funding these additional advantages is unnecessarily costly and inequitable.
It additionally makes it troublesome for conventional Medicare to compete with Medicare Benefit.
Conventional Medicare, which tends to value the Medicare program much less per enrollee, is barely allowed to offer the usual Medicare advantages package deal. If its enrollees need dental protection or listening to aids, they should buy these individually, alongside a Half D plan for pharmaceuticals and a Medigap plan to decrease their deductibles and co-payments.

AP Photograph/Pablo Martinez Monsivais
The system units up Medicare Benefit plans to not solely be overpaid but additionally be more and more well-liked, all on the taxpayers’ dime. Plans closely promote to potential enrollees who, as soon as enrolled in Medicare Benefit, will probably have issue switching into conventional Medicare, even when they determine the additional advantages should not definitely worth the prior authorization hassles and the restricted supplier networks. In distinction, conventional Medicare usually doesn’t interact in as a lot direct promoting. The federal authorities solely accounts for 7% of Medicare-related advertisements.
On the identical time, some individuals who want extra well being care and are having hassle getting it by means of their Medicare Benefit plan – and are capable of change again to conventional Medicare – are doing so, based on an investigation by The Wall Avenue Journal. This leaves taxpayers to choose up take care of these sufferers simply as their wants rise.
The place can we go from right here?
Many researchers have proposed methods to cut back extra authorities spending on Medicare Benefit, together with increasing danger adjustment audits, decreasing or eliminating high quality bonus funds or utilizing extra knowledge to enhance benchmark estimates of enrollee prices. Others have proposed much more basic reforms to the Medicare Benefit fee system, together with altering the premise of plan funds in order that Medicare Benefit plans will compete extra with one another.
Decreasing funds to plans might should be traded off with reductions in plan advantages, although projections recommend the reductions could be modest.
There’s a long-running debate over what kind of protection must be required beneath each conventional Medicare and Medicare Benefit. Just lately, coverage specialists have advocated for introducing an out-of-pocket most to conventional Medicare. There have additionally been a number of unsuccessful efforts to make dental, imaginative and prescient, and listening to companies a part of the usual Medicare advantages package deal.
Though all older folks require common dental care and plenty of of them require listening to aids, offering these advantages to everybody enrolled in conventional Medicare wouldn’t be low-cost. One method to offering these vital advantages with out considerably elevating prices is to make these advantages means-tested. This could permit folks with decrease incomes to buy them at a lower cost than higher-income folks. Nonetheless, means-testing in Medicare will be controversial.
There’s additionally debate over how a lot Medicare Benefit plans must be allowed to range. The common Medicare beneficiary has over 40 Medicare Benefit plans to select from, making it overwhelming to check plans. As an illustration, proper now, the common individual eligible for Medicare must sift by means of the high-quality print of dozens of various plans to check vital elements, resembling out-of-pocket maximums for medical care, protection for dental cleanings, cost-sharing for inpatient stays, and supplier networks.
Though tens of millions of persons are in suboptimal plans, 70% of individuals don’t even examine plans, not to mention change plans, through the annual enrollment interval on the finish of the yr, probably as a result of the method of evaluating plans and switching is troublesome, particularly for older People.
MedPAC, a congressional advising committee, means that limiting variation in sure vital advantages, like out-of-pocket maximums and dental, imaginative and prescient and listening to advantages, may assist the plan choice course of work higher, whereas nonetheless permitting for flexibility in different advantages. The problem is determining methods to standardize with out unduly decreasing customers’ choices.
The Medicare Benefit program enrolls over half of Medicare beneficiaries. Nonetheless, the $83-billion-per-year overpayment of plans, which quantities to greater than 8% of Medicare’s whole finances, is unsustainable. We imagine the Medicare Benefit fee system wants a broad reform that aligns insurers’ incentives with the wants of Medicare beneficiaries and American taxpayers.
This text is a part of an occasional sequence inspecting the U.S. Medicare system.
Previous articles within the sequence:
Medicare vs. Medicare Benefit: gross sales pitches are sometimes from biased sources, the alternatives will be overwhelming and neutral assist is just not equally out there to all![]()
Grace McCormack, Postdoctoral researcher of Well being Coverage and Economics, College of Southern California and Erin Duffy, Analysis Scientist and Director of Analysis Coaching in Well being Coverage and Economics, College of Southern California
This text is republished from The Dialog beneath a Inventive Commons license. Learn the unique article.